Abstract
Objectives: To investigate publicly funded healthcare costs according to faller status and the periods pre- and post-cataract surgeries, and identify factors associated with higher monthly costs in older people with bilateral cataract.
Methods: This prospective cohort study included community-dwelling older people aged 65 and over (between 2012 and 2019); at baseline participants had bilateral cataract and were waiting for cataract surgery in New South Wales (NSW) public hospitals. Participants were followed for 24 months. The study used self-reported and linked data (Medicare Benefits Schedule, Pharmaceutical Benefits Scheme, NSW Admitted Patient and Emergency Department Data Collections) to identify falls, cataract surgeries and healthcare costs incurred by the Australian and NSW Governments, all costs were inflated to 2018–19 Australian dollars (AUD). Median monthly healthcare costs were calculated for faller status (non-faller, non-medically treated faller, medically treated faller) and surgery periods (pre-surgery, post-first surgery, post-second surgery). Costs in the 30 days following a medically treated fall were estimated. A generalised linear model was used to investigate predictors of healthcare costs.
Results: During the median follow-up period of 24 months, 274 participants suffered 448 falls, with 95 falls requiring medical treatment. For medically treated falls, the mean cost in the 30 days after treatment was A$3779 (95% confidence interval $2485, $5074). Higher monthly healthcare costs were associated with a higher number of medications, being of the male sex, having one or more medically treated falls and having bilateral cataract surgery. After excluding the cost of cataract surgery, there were no significant differences in healthcare costs between the pre-cataract surgery, post-first eye cataract surgery and post-second eye cataract surgery periods.
Conclusions: To our knowledge, this is the first study investigating publicly funded costs related to falls and cataract surgery in older people with bilateral cataract. This information enhances our understanding of healthcare costs in this group. The patterns in costs associated with falls can guide future government healthcare expenditure on falls treatment and prevention, including timely cataract surgery.
Full text
Introduction
Falls are the most common injury-related cause of hospitalisation in Australia, with older adults (aged 65 and over) being more likely to be hospitalised due to a fall compared to other age groups.1 It is estimated that one in three older adults fall each year2, and the risk of falling increases with cataract-related vision impairment.3 First and second eye cataract surgery have been shown to reduce the risk of falls in older people with cataract.4,5 An Australian study found that the age- and sex-adjusted incidence of falls in older people scheduled for cataract surgery reduced from 1.17 to 0.81 falls per year after first eye surgery, and further decreased to 0.41 falls per year after second eye surgery.5
Fall-related injuries pose a significant burden on the healthcare system, amounting to an annual national health expenditure of $3.6 billion in 2015–16.6 Recent modelling studies suggest that expediting cataract surgery could result in health system cost savings due to the number of falls avoided.7,8 Currently, there is a paucity of real-world data on healthcare costs associated with falls experienced by those awaiting cataract surgery. The Falls in Older people with Cataract, a longitudinal evalUation of impact and riSk (FOCUS9) study, which prospectively monitored falls in older people with cataract using monthly self-reported and linked administrative health data, provides an opportunity to fill this knowledge gap.
Using administrative data, the average cost of treating fall-related injuries in Australia in 2006–07 was estimated to be $3906.10 Using self-reported data, the average cost of treating an injurious fall in 2000 was estimated to be $1600.11 In the research reported here, we synthesised self-reported and linked administrative healthcare data in a cohort of older people with bilateral cataract. Our first aim was to estimate the publicly funded costs of healthcare in the 30 days after a medically treated fall. Our second aim was to investigate the drivers of healthcare costs in this cohort, including the impact of falls. Finally, our third aim was to investigate the impact of cataract surgery on healthcare costs. A better understanding of the drivers of healthcare costs in this cohort can affect practice and policy around the provision of cataract surgery to prevent falls and promote healthy ageing in Australia.
Methods
Study design, participants and setting
This data linkage study investigated healthcare costs incurred by the Australian Government in a cohort of older people with cataract. The study drew participants from the New South Wales (NSW) cohort of the FOCUS study9 – a prospective, observational study of the impact of cataract surgery on falls, vision and quality of life. Participants included adults aged 65 and older with bilateral cataract who were on public hospital waiting lists for cataract surgery. Participants were living in the community, were able to walk, could travel for study visits and had adequate English language skills to complete study assessments. Exclusion criteria included cognitive impairment (a score of >2 errors on the Short Portable Mental Status Questionnaire) and a diagnosis of dementia, Parkinson’s disease, previous stroke or significant ocular comorbidities. This data linkage study analysed data from four public tertiary referral ophthalmology clinics in NSW (Sydney Eye Hospital, Westmead Hospital, Bankstown-Lidcombe Hospital and Royal North Shore Hospital) that were collected between December 2013 and August 2016.
FOCUS study data variables
Participants attended a baseline study visit while waiting for their first eye cataract surgery. They then attended up to two follow-up study visits, each approximately 3 months after having first and second eye cataract surgery (See Appendix Figure A1, available from: doi.org/10.5281/zenodo.10042127). Participants provided their medical history (record of current medications) and performed a vision assessment at each visit. We assessed logarithm of the minimum angle of resolution (logMAR) visual acuity using an Early Treatment Diabetic Retinopathy Study chart at 3 m. We measured contrast sensitivity using the Mars letter contrast sensitivity test at 50 cm (normal range: 1.52–1.72 log units).
Participants prospectively self-reported falls using monthly calendars from the baseline study visit for 24 months, or up until 6 months after their second eye cataract surgery. A fall was defined as an unexpected event in which participants came to rest on the ground, floor or lower level.12 We followed up any reported falls with a telephone call to determine the circumstances of the fall, if there was any resulting injury and if medical intervention was sought (e.g. general practitioner [GP] visit, emergency department [ED] presentation, hospital admission). If a completed calendar was not received, we telephoned the participant to collect falls data.
The Department of Health Human Research Ethics Committee (Project 36/2014) and NSW Population and Health Services Research Ethics Committee (approval number 2013/04/458) both approved this study. We obtained written informed consent from participants to link FOCUS study records with administrative health datasets. This research was supported by a National Health and Medical Research Council Project Grant (APP1048302).
Administrative health data linkage, data variables and cost estimation
The Centre for Health Record Linkage (CHeReL) used probabilistic linkage methods to perform data linkage with hospital administrative datasets, the NSW Admitted Patient Data Collection (APDC) and the Emergency Department Data Collection (EDDC).13 Participant identifiers supplied for data linkage, date ranges and the data variables extracted are presented in Appendix Table A1 (available from: doi.org/10.5281/zenodo.10042127). The NSW APDC records all admitted patient services provided by public and private hospitals and private day procedure centres, and the NSW EDDC records all patient presentations to public hospital EDs. We identified falls based on the principal and additional diagnoses in the APDC data using the International statistical classification of diseases and related health problems, tenth revision, Australian modification codes (Appendix Table A2, available from: doi.org/10.5281/zenodo.10042127), and the principal diagnosis in the EDDC data using the Systematized Nomenclature of Medicine Clinical Terms (Appendix Table A3, available from: doi.org/10.5281/zenodo.10042127).
Hospitalisation and ED costs were based on data from the National Hospital Cost Data Collection (NHCDC) public sector report for years 2013–14 to 2018–19.14 We calculated hospitalisations costs by multiplying the average cost of admitted patient separations (excluding ED costs) with the linked data cost weight supplied by CHeReL. Cost weights are a measure of the relative cost of an episode of care in hospital, with the average cost assigned a weight of 1. For ED presentations, we used the average cost of admitted or non-admitted ED separations from the NHCDC report.14
Services Australia performed data linkage with the Medicare Benefits Schedule (MBS) and Pharmaceutical Benefits Scheme (PBS). The MBS captures usage of Australian Government-subsidised health professional services provided to private patients, such as visits to the GP, medical specialists, pathology services, some allied health services and hospital services. The PBS captures dispensing of government-subsidised prescription medicines to eligible private patients at community pharmacies and hospital pharmacies. Participant identifiers supplied for data linkage, date ranges and the data variables extracted are shown in Appendix Table A1 (available from: doi.org/10.5281/zenodo.10042127). We extracted the MBS benefit paid and net PBS benefit for the cost calculations.
Data analysis and statistical methods
We prepared the data before analysis (described in the Appendix Box A1). We performed the statistical analysis using IBM SPSS Statistics Version 26 and GraphPad Prism 9 for Windows 64-bit (Version 9.3.0). We used descriptive statistics to summarise participant age and medical and vision characteristics.
Aim 1. Estimate healthcare costs in the 30 days after a fall
Falls were self-reported (FOCUS study) or identified in the APDC/EDDC datasets using fall-related diagnosis codes. Falls were categorised as either non-medically treated or medically treated. Medically treated falls were further categorised according to the record of treatment: GP visit, ED presentation or hospital admission. If a fall resulted in an ED presentation and hospital admission, it was categorised as a hospital admission. Healthcare costs incurred by the Australian and NSW Governments were estimated using linked data (MBS and PBS benefits, cost of hospital admissions and ED presentations). Costs were adjusted for health inflation to the financial year 2018–1915 and expressed in AUD. All costs (not restricted to falls-specific care) incurred in the 30 days after a medically treated fall (starting from the date of the fall) were included in the analysis. Falls with missing linked data were excluded. To prevent duplication of costs, when multiple falls occurred within 30 days of the first fall, the costliest period was selected for analysis. As this research focused on direct expenditure from a health system perspective, it did not account for indirect costs or out-of-pocket patient costs.
The Shapiro–Wilk test was used to examine if variables were normally distributed. Median (Q1–Q3) costs were reported when the distribution of costs was non-normal. Mean costs (95% confidence interval, CI) were also provided to allow comparison with previously published estimates.
Aim 2. Investigate faller status and other drivers of healthcare costs
Participants were categorised as non-fallers (i.e. no falls during the study period), non-medically treated fallers (i.e. ≥1 fall, with none requiring medical attention) or medically treated fallers (i.e. ≥1 fall requiring medical intervention during the study period). The average monthly (30.4 days) healthcare costs (MBS, PBS, hospital emergency and admission) incurred during the FOCUS study period were calculated for each participant and compared across faller status groups. Comparisons between faller groups were performed using the chi-square test and Kruskal–Wallis test, with post-hoc pairwise comparison adjusted by the Bonferroni correction for multiple comparisons. A p value < 0.05 was considered significant.
A generalised linear model (model type: gamma with log link) was used to identify predictors of healthcare costs, including age, number of medications at baseline study visit, sex, faller group and number of cataract surgeries undertaken during the FOCUS study period. Estimated marginal means were used to estimate mean costs by sex, faller group and number of cataract surgeries.
Aim 3. Investigate healthcare costs according to cataract surgery periods
The effect of cataract surgery on healthcare costs was examined by comparing three study periods: before first eye surgery, between first and second eye surgery, and after second eye surgery. To robustly assess the impact of surgery, this analysis was restricted to participants who were observed during all three periods (i.e. progressed to second eye surgery). This analysis includes linked data that precede FOCUS study entry and follow-up data that postdate FOCUS study exit. Participants with missing linked data were excluded from the analysis.
To account for different exposure lengths, particularly between first and second eye surgery compared to other periods, the healthcare cost per month (30.4 days) was calculated for analysis. Costs were compared over three exposure periods using the Friedman’s two-way analysis of variance by ranks test.
Results
Participant characteristics
Of the 304 participants who consented to take part in the study (Appendix Figure A1, available from: doi.org/10.5281/zenodo.10042127), 30 participants were excluded from the analysis because records were returned with no linked data (n = 22), there were incorrectly linked data (cataract surgery predated study enrolment, n = 4) or FOCUS follow-up data were missing (n = 4).
Of the remaining 274 participants, 151 (55.1%) were female and most were living alone (72.0%). At baseline, the median age of participants was 75 years (Q1–Q3: 71–79). Most were retired and receiving the age pension (87%).
Cataract-related vision impairment at baseline was variable among participants. On average, there was mild vision impairment, with median binocular logMAR visual acuity of 0.24 (Q1–Q3: 0.10–0.40) and binocular contrast sensitivity of 1.52 log units (Q1–Q3: 1.40–1.68).
During the median observation period of 24 months (Q1–Q3: 19–24), 34 participants (12.4%) did not progress to cataract surgery (Appendix Figure A1, available from: doi.org/10.5281/zenodo.10042127). Of the participants who did have surgery, 240 (87.6%) had first eye cataract surgery and 160 (58.4%) had second eye cataract surgery.
Table 1. Characteristics of participants according to faller status
| Characteristics | Non-faller (n = 119) |
Non-medically treated faller (n = 103) |
Medically treated faller (n = 52) |
p value |
| Baseline age, median (Q1–Q3), years | 75 (71–79) | 75 (71–79) | 77 (72–81) | 0.135a |
| Medications, median (Q1–Q3), n | 4 (1–6) | 4 (2–7) | 4 (2–7) | 0.487a |
| Baseline binocular VA, median (Q1–Q3), logMAR | 0.24 (0.12–0.42) | 0.20 (0.08–0.36) | 0.24 (0.11–0.43) | 0.464a |
| Baseline binocular CS, median (Q1–Q3), log units | 1.44 (1.40–1.68) | 1.56 (1.44–1.68) | 1.44 (1.36–1.64) | 0.126a |
| Sex | ||||
| Female, n (%) | 67 (56%) | 55 (53%) | 29 (56%) | 0.905b |
| Male, n (%) | 52 (44%) | 48 (47%) | 23 (44%) | – |
| Cataract surgeriesc | ||||
| None, n (%) | 18 (15%) | 11 (11%) | 12 (23%) | 0.191b |
| One, n (%) | 39 (33%) | 44 (43%) | 19 (37%) | – |
| Two, n (%) | 62 (52%) | 48 (46%) | 21 (40%) | – |
VA = visual acuity; CS = contrast sensitivity
Note: Characteristics are for 274 participants.
a The p value was calculated using the Kruskal–Wallis test.
b The p value was calculated using the chi-square test.
c Includes the number of cataract surgeries undertaken during the FOCUS study period.
Healthcare costs in the 30 days after a fall
During the FOCUS study, participants experienced 448 falls, including 353 (78.8%) non-medically treated falls. There were 95 (21.2%) medically treated falls, which involved either a GP visit (n = 49, 10.9%), ED presentation (n = 12, 2.7%) or hospital admission (n = 34, 7.6%). In total, 9 (2.0%) falls resulted in a fracture. After excluding falls with missing linked data (n = 11), falls occurring outside Australia (n = 1), recurrent falls within 30 days of another fall (n = 8) and non-medically treated falls, there were 75 medically treated falls that were included in the analysis.
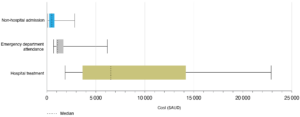
In the 30 days after a medically treated fall (n = 75), the median healthcare cost was estimated to be $1015 (Q1–Q3: $400–$5396) and the mean cost was estimated to be $3779 (95% CI $2485, $5074). Healthcare costs following a fall that required hospital admission (n = 27), ED attendance (n = 7) or non-hospital treatment (n = 41) were significantly different from each other (p < 0.001, Kruskal–Wallis test; Figure 1). In the 30 days after a hospital admitted fall, the median healthcare cost was $6524 (Q1–Q3: $3643–$14 184) and the mean cost was $9068 (95% CI $6473, $11 663). Following an emergency department treated (non-admitted) fall, the median cost was $1095 (Q1–Q3: $972–$1698) and the mean cost was $1870 (95% CI $76, $3664). Following a non-hospital treated fall, the median cost was $494 (Q1–Q3: $257–$771) and the mean cost was $623 (95% CI $447, $799).
Figure 1. Healthcare costs incurred by Government associated with either hospital admitted (n = 27), emergency department attended (n = 7) and non-hospital treated falls (n = 41) (click figure to enlarge)
Costs were significantly different across the three groups (Kruskal-Wallis, p < 0.0001).
Whiskers represent range (minimum, maximum).
Costs are reported in AUD for the 2018-19 financial year.
Healthcare costs according to participant characteristics
There were 119 (43%) participants in the non-faller group, 103 (38%) participants in the non-medically treated faller group and 52 (19%) participants in the medically treated faller group. The baseline age, number of medications, visual acuity and contrast sensitivity were not significantly different between the faller groups (p > 0.05, Kruskal–Wallis test; Table 1). Similarly, there was no significant association between the faller group and sex or number of cataract surgeries (p > 0.05, chi-square test).
Median monthly healthcare costs over the 24-month follow-up period were significantly different across the three faller groups (p = 0.022, Kruskal–Wallis test; Table 2). Post-hoc analysis showed that the median healthcare costs for the non-faller and medically treated faller groups were significantly different from each other (p = 0.022, pairwise comparison with Bonferroni correction), but neither were significantly different from non-medically treated fallers (p = 1 and p = 0.06, respectively).
Table 2. Median monthly healthcare costs according to faller status
| Costs per month, median (Q1–Q3) | Non-faller (n = 119) |
Non-medically treated faller (n = 103) |
Medically treated faller (n = 52) |
p valuea |
| PBS-subsidised medicines, $ | 83 (29–156) | 69 (29–128) | 77 (35–165) | 0.693 |
| MBS-subsidised services, $ | 170 (101–269) | 174 (101–283) | 206 (135–320) | 0.144 |
| ED attendances, $ | 0 (0–41) | 0 (0–40) | 42 (21–109) | 0.083 |
| Hospital admissions, $ | 238 (0–477) | 238 (0–487) | 403 (113–869) | <0.001 |
| Total monthly cost, $ | 529 (286–812) | 511 (317–921) | 895 (346–1499) | 0.022 |
PBS = Pharmaceutical Benefits Scheme; MBS = Medicare Benefits Schedule; ED = emergency department
Note: All cost figures are in Australian dollars.
a The p value was calculated using the Kruskal–Wallis test.
After adjusting for covariates, a generalised linear model (Appendix Table A4, available from: doi.org/10.5281/zenodo.10042127) showed that participants who had medically treated falls had higher monthly healthcare costs (estimated marginal mean of $1017) than those who had non-medically treated falls ($753) and those who did not fall ($722) (Appendix Table A5, available from: doi.org/10.5281/zenodo.10042127). Other significant associations included being of the male sex (estimated marginal means: $928 for males and $726 for females) and having more than one cataract surgery during the study period (none: $675, one: $873 and two: $938).
Healthcare costs according to cataract surgery periods
Of the 160 participants who progressed to second eye surgery (Appendix Figure A1, available from: doi.org/10.5281/zenodo.10042127), 26 were missing MBS or PBS linked data from the period post-second eye surgery so were excluded from the analysis. For the remaining 134 participants, the median monthly healthcare costs were significantly different across the three surgery periods (p < 0.001, Friedman’s two-way analysis of variance by ranks test, χ2(2) = 53.746; Table 3). When cataract surgery costs were excluded, the differences between the three periods were no longer statistically significant (p = 0.130, χ2(2) = 4.075).
Table 3. Healthcare costs per month for three cataract surgery periods
Note: Figures are for participants who had surgery in both eyes during the study period and had complete data (n = 134).
a For this analysis, median days observed before first eye surgery was 365 days (Q1-Q3:365-365); between first and second eye surgery was 223 days (127-346) and after second eye surgery was 351 days (194-365).
b The p value was calculated using Friedman’s two-way analysis of variance by ranks test.
Discussion
Using self-reported and linked administrative data, this study provided a robust estimate of healthcare costs in older adults with cataract who undergo cataract surgery in public hospitals in Australia. To our knowledge, this is the first cohort study that investigated healthcare costs in participants across three exposure periods: before first eye cataract surgery, between first and second eye cataract surgery, and after second eye cataract surgery. After excluding cataract surgery costs, there was no significant difference in healthcare costs across the three periods. Additionally, we found that in this cohort, people who had a medically treated fall, had a higher number of prescription medications and were of male sex had the highest government-incurred healthcare costs.
These findings contribute to the understanding of the costs of falls in older people with cataract to the healthcare system. Previous studies conducted in Australia have used prospective falls data collection11 and administrative health data10 to estimate the average cost of medically treated falls to be $1600 (in the year 2000) and $3906 (in the year 2006–07), respectively. In this study, we used data linkage to estimate the average healthcare cost in the 30 days following a medically treated fall to be $3779 (in the financial year 2018–19). Due to differences in methodology, results from this study are not directly comparable to previous studies.10,11,16 As this study included all healthcare costs in the 30 days following a fall, not all costs were specific to falls. Previous studies10,16 have also included additional costs that were not accounted for in this study, such as discharge to residential aged care, so this precluded direct comparison of calculated costs.
Data linkage is a highly cost-effective method for measuring the cost of cataract-related falls. However, routinely collected hospital data may not always be accurately collected and coded (with respect to primary diagnosis and main procedure code)17, and it was not possible to comprehensively validate this data. Some instances of medically treated falls were missing linked data records that corroborated self-reported data, which meant that they had to be excluded from cost analyses. Compared to other studies using data linkage, the sample size for this study was small. As this study was designed to examine direct healthcare costs incurred by governments, it did not account for health gains or improvements in quality of life associated with cataract surgery, nor did it account for participant out-of-pocket costs or indirect costs (e,g, lost productivity) associated with accessing care or recovering from a fall.
Globally, cataract surgery has been shown to improve quality of life and be a cost-effective procedure.18,19 However, due to barriers to accessing surgery, cataract remains a leading cause of vision impairment.20 In this study, the median waiting time for first and second eye surgery was 224 days and 343 days, respectively. The true waiting time for first eye surgery was likely longer, as participants were recruited from hospital waiting lists and had likely already served a waiting period for an outpatient assessment in order to be placed on a surgical wait list.8,21 Previous studies of the FOCUS cohort have shown that while waiting for cataract surgery, people are at greater risk of falls and related injuries, depressive symptoms and a reduced quality of life.4,22,23 This study did not find a significant change in healthcare costs following first and second eye cataract surgery (when the cost of surgery was excluded). As not all participants progressed to second eye surgery during the study, a longer follow-up period may have led to different results. However, this study did demonstrate the high costs associated with falls in this cohort, who have 2–3 times the odds of falling compared to people without cataract.3 This highlights the need to increase falls prevention efforts, of which timely cataract surgery and appropriate post-surgical refractive correction are an important part.24
Conclusion
Falls are frequent among older people awaiting cataract surgery, and in this study, about 1 in 5 falls required medical treatment (21.2%). People who suffered medically treated falls had significantly higher healthcare costs than non-fallers. The findings from this study may help guide future healthcare spending decisions by governments, including the funding of timely cataract surgery to prevent falls and avoid fall-related treatment costs.
Peer review and provenance
Externally peer reviewed, not commissioned.
Copyright:
© 2023 Huang-Lung et al. This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International Licence, which allows others to redistribute, adapt and share this work non-commercially provided they attribute the work and any adapted version of it is distributed under the same Creative Commons licence terms.
References
- 1. Australian Institute of Health Welfare. Falls. Canberra: AIHW; 2022 [cited 2022 Sep 12]. Available from: www.aihw.gov.au/reports/injury/falls
- 2. Salari N, Darvishi N, Ahmadipanah M, Shohaimi S, Mohammadi M. Global prevalence of falls in the older adults: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2022;17(1):334. • CrossRef | PubMed
- 3. McCarty CA, Fu CL, Taylor HR. The risks of everyday life: predictors of falls in the Melbourne visual impairment project. Aust N Z J Public Health. 2002;26(2):116–9. CrossRef | PubMed
- 4. Harwood RH, Foss AJ, Osborn F, Gregson RM, Zaman A, Masud T. Falls and health status in elderly women following first eye cataract surgery: a randomised controlled trial. Br J Ophthalmol. 2005;89(1):53–9. CrossRef | PubMed
- 5. Keay L, Ho KC, Rogers K, McCluskey P, White AJ, Morlet N, et al. The incidence of falls after first and second eye cataract surgery: a longitudinal cohort study. Med J Aust. 2022;217(2):94–9. CrossRef | PubMed
- 6. Australian Institute of Health and Welfare. Injury expenditure in Australia 2015–16. Canberra: AIHW; 2020 [cited 2022 Sep 12]. Available from: https://www.aihw.gov.au/reports/health-welfare-expenditure/injury-expenditure-in-australia-2015-16
- 7. Boyd M, Kvizhinadze G, Kho A, Wilson G, Wilson N. Cataract surgery for falls prevention and improving vision: modelling the health gain, health system costs and cost-effectiveness in a high-income country. Inj Prev. 2020;26(4):302–9. CrossRef | PubMed
- 8. Huang-Lung J, Angell B, Palagyi A, Taylor HR, White A, McCluskey P, et al. The true cost of hidden waiting times for cataract surgery in Australia. Pub Health Res Pract. 2022;32(3):31342116. CrossRef | PubMed
- 9. Keay L, Palagyi A, McCluskey P, Lamoureux E, Pesudovs K, Lo S, et al. Falls in Older people with Cataract, a longitudinal evalUation of impact and riSk: the FOCUS study protocol. Inj Prev. 2014;20(4):e7. CrossRef | PubMed
- 10. Watson WL, Clapperton AJ, Mitchell RJ. The cost of fall-related injuries among older people in NSW, 2006–07. N S W Public Health Bull. 2011;22(4):55–9. CrossRef | PubMed
- 11. Tiedemann AC, Murray SM, Munro B, Lord SR. Hospital and non-hospital costs for fall-related injury in community-dwelling older people. N S W Public Health Bull. 2008;19(9–10):161–5. CrossRef | PubMed
- 12. Lamb SE, Jorstad-Stein EC, Hauer K, Becker C, Prevention of Falls Network Europe, Outcomes Consensus Group. Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53(9):1618–22. CrossRef | PubMed
- 13. Irvine K, Hall R, Taylor L. A profile of the Centre for Health Record Linkage. In J Popul Data Sci. 2019;4(2):1142. CrossRef | PubMed
- 14. Independent Health and Aged Care Pricing Authority. National Hospital Cost Data Collection public sector report. Sydney, Australia: IHACPA; 2023 [cited 2023 Oct 24]. Available from: www.ihacpa.gov.au/health-care/costing/national-hospital-cost-data-collection/national-hospital-cost-data-collection-public-sector
- 15. Australian Institute of Health Welfare. Health expenditure Australia 2019–20. Canberra: AIHW; 2021 [cited 2022 Sep 12]. Available from: https://www.aihw.gov.au/reports/health-welfare-expenditure/health-expenditure-australia-2019-20
- 16. Hendrie D, Hall SE, Arena G, Legge M. Health system costs of falls of older adults in Western Australia. Aust Health Rev. 2004;28(3):363. CrossRef | PubMed
- 17. Burns EM, Rigby E, Mamidanna R, Bottle A, Aylin P, Ziprin P, et al. Systematic review of discharge coding accuracy. J Public Health (Oxf). 2012;34(1):138–48. CrossRef | PubMed
- 18. Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007;114(9):1670–8. CrossRef | PubMed
- 19. Brown GC, Brown MM, Menezes A, Busbee BG, Lieske HB, Lieske PA. Cataract surgery cost utility revisited in 2012: a new economic paradigm. Ophthalmology. 2013;120(12):2367–76. CrossRef | PubMed
- 20. Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health. 2021;9(4):e489–e551. CrossRef | PubMed
- 21. Do VQ, McCluskey P, Palagyi A, Stapleton FJ, White A, Carnt N, et al. Are cataract surgery referrals to public hospitals in Australia poorly targeted? Clin Exp Ophthalmol. 2018;46(4):364–70. CrossRef | PubMed
- 22. Palagyi A, Keay L, Rogers K. Depressive symptoms in older adults awaiting cataract surgery: methodological and statistical issues – response. Clin Exp Ophthalmol. 2017;45(8):841–2. CrossRef | PubMed
- 23. Palagyi A, McCluskey P, White A, Rogers K, Meuleners L, Ng JQ, et al. While we waited: incidence and predictors of falls in older adults with cataract. Invest Ophthalmol Vis Sci. 2016;57(14):6003–10. CrossRef | PubMed
- 24. Palagyi A, Morlet N, McCluskey P, White A, Meulener L, Ng JQ, et al. Visual and refractive associations with falls after first-eye cataract surgery. J Cataract Refract Surg. 2017;43(10):1313–213. CrossRef | PubMed